Katrina Nevin
Labor
I had planned very carefully and excitedly for a home birth. After swimming in the ocean before lunch I began to feel light contractions. John came home from work on the ferry and rode home fast on his bicycle and by 3:30 things had really accelerated. Contractions were coming every 2 minutes and my beautiful birth team was by my side.

Leia listened to the baby’s heartbeat, Meg inflated the tub, Fallon helped me sip water and John helped me to breath. Outdoors the woodpeckers fed their babies and the tall green grass swayed in the breeze. I was full of confidence and gratitude. The baby’s heartbeat sounded like the same happy techno beat I’d heard throughout pregnancy, like a distant dance party heard across some hills, boom boom boom boom. Time passed beautifully and I took a rest and breathed more deeply knowing that everything was good.

Around 6:15 Leia listened to the heartbeat yet again and it was instantly clear that something was very, very wrong. The disco party sounded like it was coming from underwater and was so, so slooow. Fa-booom fa-boom fa-boooom. Leia called for oxygen, Meg got the tank, John brought the car onto the lawn, Fallon found me a skirt. Then we were in the car, me breathing oxygen and panting in the back seat while Leia held the Doppler and the heartbeat was so slow and Meg called the emergency room and John forced himself to drive responsibly. Fa-boom fa-boom fa-boom. Into the hospital barefoot and laboring. Then everything is a blur of pain and confusion and hearing the heartbeat and asking in my head over and over why? Why? Why? No no no this wasn’t the plan.
The baby's heart rate was still extremely slow we got to the MV hospital but the doctor spent an hour trying to continue a monitored labor because the heart rate kept periodically going back up. I don’t really remember that hour very well because the contractions were so intense and constant that everything was a blur. Finally the doctor attempted to put a fetal monitor directly on the baby's head through my partially dilated cervix. When she did that she broke the amniotic sack and the liquid that trickled out was a dark, dark brown. Bad. Very, very bad. Brown amniotic fluid means that blood and poop (meconium) were in the uterus and the baby was swallowing that and getting it into her lungs. We found out later that my placenta had separated from the uterine wall some time during early labor (this is called a placental abruption) so in addition to my baby not getting enough oxygen from the damaged placenta my uterus was also filling up with blood which the baby was swallowing. That's when they decided to do an emergency C-section and rushed me into surgery.
Surgery: What an emergency C-section is really like
All this time I had been having fast, hard contractions but when they moved to the operating room they gave me a drug to stop the contractions so that they could perform the surgery on muscles that weren’t constantly squeezing. The impact of this drug on me was that in addition to painful rip roaring contractions I was suddenly shaking uncontrollably as the drug tried to stop my body from being in labor. Awesome. I was wheeled into the OR and the anesthesiologist looked down at me over his mask and said “I’m doctor Patel, I’ll take care of you.” And that’s all I remember of that.
When I woke up from the surgery I remember having an immediate sensation of relief, I felt so relaxed and rested. Then a voice said “Can you wiggle the fingers of your left hand for me? How about your right?” and I suddenly became horribly aware that not only could I not wiggle my fingers I also couldn’t breath! I tried to take a breath and nothing happened, I tried to speak or call out to say “I can’t breath!” and nothing happened. I was drowning in air and I couldn’t tell anyone! Then all at once (or so it seemed to me) I miraculously could breath again and I was being wheeled out of the OR and back up to maternity.
I wish someone had explained to me in that moment what was happening. It was a very simple thing but I didn’t get an explanation until I asked a nurse about it later that night. I wish I'd known I was on a breathing tube! Just in case you ever find yourself needing emergency anesthesia for any kind of surgery keep this story in mind. I had been intubated during the C-section and I didn't know it. That means that there was breathing tube that went down my throat and into my lungs. When they reduced the anesthesia to wake me up they left the breathing tube in place until they knew that I had awoken sufficiently to be able to breath on my own. Then they removed the tube in my throat. So when I awoke there was a machine breathing for me and I couldn't physically take my own breaths until they removed that tube. This was a horribly frightening experience and I wish someone had told me what was going on in the moment so I didn't think I was suffocating.
Another thing I wish I had known to expect was the seizing, shooting pain in my neck and shoulders in the 48 hours following emergency surgery. It was worse by far than the pain of my incision, (which was excruciating) and I couldn’t move or stretch my muscles out, all I could do was sit propped up uncomfortably in bed feeling like I'd been slung around like a whiplash victim. Apparently for safety they have to strap your arms out to the sides like Jesus on the cross when you go under general anesthesia. Being restrained in this unnatural pose for over an hour frequently results in excruciating neck and shoulder pain for all types of emergency surgery patients. I'm not sure what they could do differently to prevent this from happening, perhaps just handle their patient more gently, but I wish I had known at the time why I was in such pain.

My baby was born blue and unresponsive. She was not breathing and she had inhaled/swallowed so much blood and meconium that her lungs were full of fluid. After being revived she was airlifted off the Island that night up to Massachusetts General Hospital (MGH) in Boston where she would spend the next 5 weeks in the Neonatal Intensive Care Unit (NICU) recovering from substantial and extensive damage to her lungs, kidneys and heart from the oxygen deprivation and meconium aspiration. By some miracle she had no damage to her brain and she recovered fully and has no evidence of her trauma except a small scar on her neck from where they put her on a lifesaving blood oxygenating machine (called ECMO) for three days while her lung tissue recovered.

Recovery in the first 48 hours
I had planned to be recovering from a natural birth at home in my own bed with my baby by my side. Instead I was recovering from major abdominal surgery in a hospital bed that was eleven floors above my baby’s room in the NICU. I never anticipated the kind of round the clock pain and exhaustion of a C-section. The mechanical hospital bed was a huge help, I don’t know how I would have gotten myself in and out of bed without being able to slowly raise my torso to a sitting position first. The first night after surgery I don’t think I slept at all. There were shooting pains in my neck and shoulder from being strapped down while under anesthesia. I was terribly thirsty but my neck was so seized up with pain that it hurt just to tilt my head back or swallow. I couldn’t laugh or cough without feeling like I was being violently sliced in half at the incision. They put compression booties on my feet overnight to keep the blood flowing and while I was soothed by the rhythmic pressure on my feet, the sighing snoring sound of the machine compressing and releasing the cuffs was hard to sleep through.
The next morning the nurses removed my catheter which didn’t hurt but was a strange sensation like needing to pee really hard for a second. Then they wanted me to try getting out of bed and sitting in a chair. The process of levering myself slowly onto my side and then lowering my legs off the bed and getting into a sitting position was monumentally difficult. Once I made it to the chair I just stayed there until it was time to get onto the gurney to be taken down to the ambulance to be transported up to Boston to join my baby.
The Ambulance ride was hell. I had no idea that our state roads were so bumpy. I spent the 45 minute ferry boat ride peacefully sleeping and then I spent the hour and a half long drive lying flat on my back on the stretcher watching the sky and trees flash by outside and trying not to tense my stomach muscles. Every single tiny bump felt like an assault, like being thrown violently against a knife. Half way through the journey I needed to pee which meant stopping the ambulance and getting off the stretcher to haphazardly squat over a commode. Pee went everywhere as I was completely focused on trying to stay upright and not use my abdominal muscles.
That night I got a nurse to wheel me down stairs eleven floors to see my baby for the first time in almost 24 hours. Standing by her bed was the first time that I didn’t notice any of my own pains. For the first week my husband pushed me everywhere in a wheelchair and wouldn’t let me walk more than was absolutely necessary. I found it hard to accept my new limitations but the pain was a constant reminder that I was not myself. There was a strange empty flapping feeling to my belly, like a bowl full of jelly being tossed around with every movement. I was surprised by how gross my post-birth body felt. I moved like a very old woman, hunched, slow, shuffling, trying to conserve energy and limit any jolts or jostles. I would shuffle to the bathroom and sit over the commode waiting to poop, and fearing to poop. The nurses wanted to see whatever came out of me for the first 48 hours so I wasn’t permitted to flush. It was mortifying and made me feel like a very unwell person, like a patient suffering from some illness instead of a new mother.

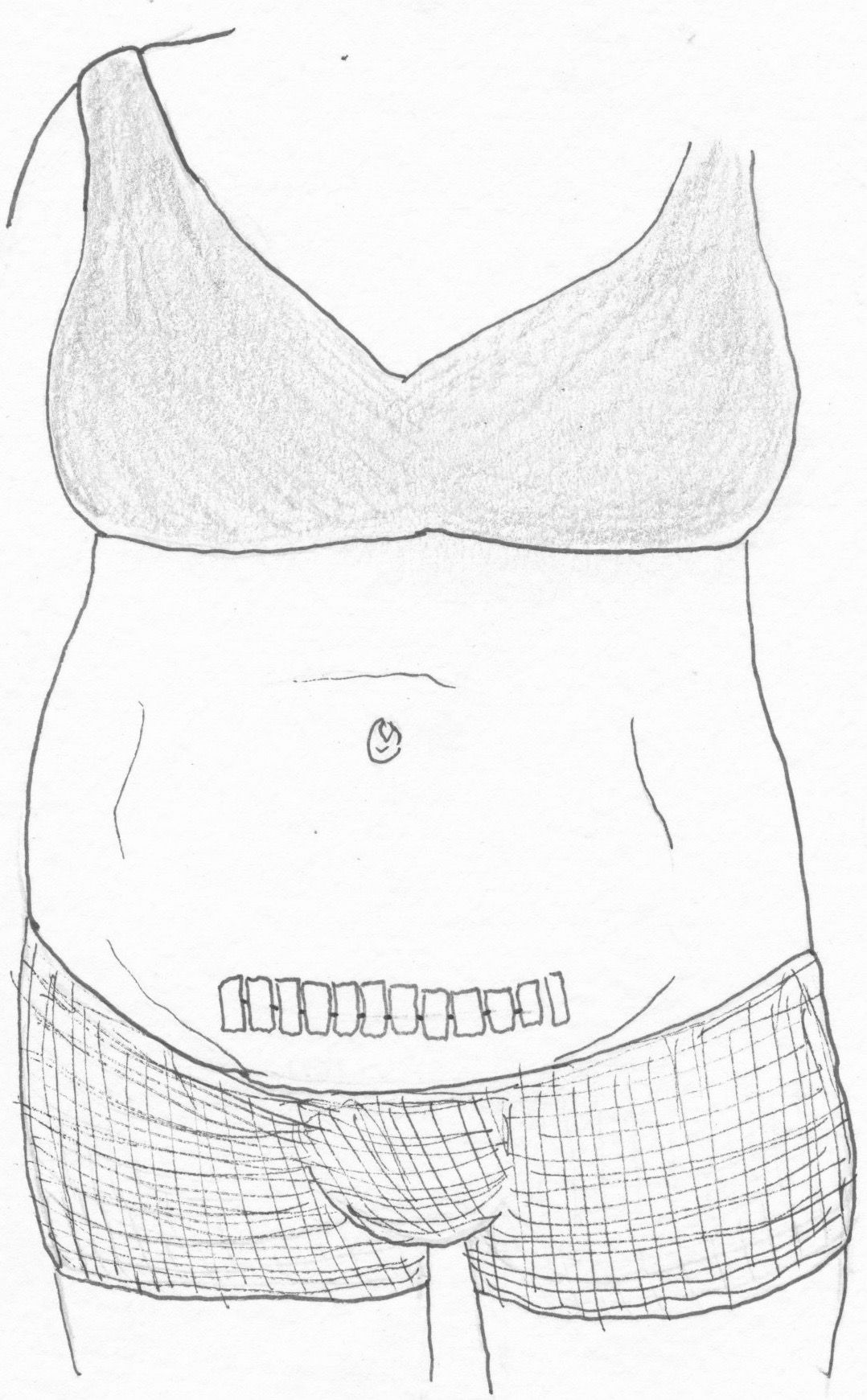
Betadine Allergy Rash
On the third day, on top of all these normal surgery pains, I developed a nasty rash reaction to the Betadine scrub they had used during surgery. Surgeons cover the area they are going to cut with a layer of Betadine before they begin surgery in order to prevent infection and kill bacteria. After they had stitched everything back up they left the Betadine on my skin. This is common practice, but it had huge ramifications for me in the days that followed.Two days after my surgery I was able to stand up and move around a bit so I took a hot shower for the first time and I carefully washed off all the yellow/brown staining from the Betadine. Three hours later I noticed a red rash starting to appear all over my abdomen, from the incision upward to above my belly button and around the sides of my waist. A couple hours after that I noticed that the rash was itchy. Shortly thereafter I was in a world of pain. I've had really bad poison ivy and poison oak rashes. This was like that but ten times worse because of the location surrounding a tender healing incision. None of the doctors or nurses caring for me recognized my symptoms or had ever encountered this problem.

I mentioned it to several of the nurses caring for my baby in the Neonatal Intensive Care Unit (NICU) and after showing the rash to them somebody said “oh yeah that’s a Betadine allergy”. Several of them had experienced the same thing after their own babies were born. It turns out that a substantial portion of the population gets a contact dermatitis allergy from Betadine, but nobody mentioned this possibility to me so when it appeared I had no idea what it was or how to treat it.
I was in a huge amount of pain, the incision from my surgery felt like it was being re-opened and my skin was extremely tender and horrifically itchy at the same time. Touching it hurt. My clothes brushing lightly against my skin as I moved hurt. Itching it hurt but also perversely made it feel better. I set about treating it as I would treat poison Ivy, with a combination of Cortizone cream, Aloe and cold compresses. None of it helped. The Cortizone cream actually seemed to inflame it more as though the steroid was irritating the rash. After a day of shellacking my skin with Aloe gel I took a cool shower. As I painfully peeled off the layers of sticky gel and cream I realized that all I had been doing was capping the rash with an impermeable barrier that didn't allow my skin to breath. I researched online and began applying a diluted solution of apple cider vinegar to my skin. This left me feeling slightly better but made me smell like a pickle.
Luckily the next morning I was back in my babies room in the NICU and a new nurse said “oh have you tried breast milk? Breast milk fixes everything.” Strange as it sounded I was desperate so I took some of the milk I'd just pumped and dabbed it all over my skin and I immediately felt relief! That whole night and day I applied my milk to the rash multiple times and the transformation was incredible. From angry red welts that were raised up and looked almost neon red, the rash faded to a muted pink glow that resembled a slight sunburn. The itching disappeared literally overnight.
I wish I could shout this piece of hard learned knowledge into the home of every single human being on this planet, but especially pregnant women because it would have saved me so much discomfort and distress if someone had just given me this information immediately after my C-section. To be on the safe side you need to use cool water and rinse that yellow stain off your skin as quickly as possible to avoid having a reaction. I had it on me for around 30 hours and it was really, really bad. Not everybody will have a reaction and some women I talked to seemed to have less extreme reactions than me, maybe they showered sooner than I did or maybe I'm just extra sensitive.
Recovery: The First Weeks After Surgery
Five days post surgery I was discharged from the hospital and we went to stay at my in-law’s house half an hour away. I was now able to walk slowly but fairly easily and squat to pick things up off the ground. Bending over at the waist was completely out of the question for several weeks. Getting in and out of bed was still a challenge but it was getting easier every time. I was starting to be able to find comfortable positions to sleep in. Unfortunately our bedroom at my in-laws was on the third floor and required going up and down 36 steps to get to and from bed every day. Steps were really hard, I felt out of breath and in pain every time I went up or down. Despite my husbands careful attention to using the wheelchair I definitely overdid it physically in the first few weeks after my surgery. The bleeding discharge was much heavier and lasted a lot longer than it might have if I had been able to go back to my home and had my baby beside me in bed instead of climbing steps, riding elevators and commuting by car too and from her hospital room every day for six weeks. My advice is to be as gentle with yourself as you possibly can be and take all the help you can get!
The incision itself healed up just fine though I was surprised by how long it took for the steri strips to come off the scar. Steri strips are the glue tape that goes on over your C-section incision to keep the stitches in place and hold everything together while the scar heals. The Doctors say you can gently pat the area of your incision with a washcloth when you shower, but not to scrub at it, or soak the area for the first week. Everyone said to me that the strips would fall off on their own after about 10 days. Mine didn't. My belly was still so big that I couldn't see my incision unless I stood in front of a full length mirror and leaned back. I wasn't sure where the ends of the actual cut were since the strips go beyond the edges of the incision and it was very creepy for me to touch the area and feel only numbness above the scar and only hard tacky glue strips on top of the scar. I was worried the stitches weren't healed so I waited two weeks and then a bit longer and still the steri strips were perfectly glued in place. They were getting really dirty from sweater lint and fuzz and they looked terrifying but I wasn't able to pick them off because it felt like I was peeling my skin off every time I tried. Finally I got into a tub and soaked until they just slipped off easily.

The Scar: Numbness
I wasn't prepared for the odd numb sensation above my scar, it felt like my hand had fallen asleep and I was touching someone else stomach, that's how little feeling their was. The lack of feeling only extended about an inch and a half above the scar but it was very strange. Around four months after my surgery the numbness above my scar finally began to fade away. But I talked to a nurse in the NICU who told me that she was still numb around her scar for one year postpartum and I’ve heard that for some people the feeling never completely comes back (especially after multiple C-sections) so just be aware that results really vary from person to person and try not to think about it too much.

Breastmilk, Breast Pumps and Feeding
Because of her traumatic birth my baby needed to be intubated and tube fed and she was not able to take any food by mouth for the first three weeks. The morning after she was born I was introduced to a breast pump. I had never even thought about pumping milk, I assumed I would be breastfeeding my baby. It quickly became apparent to me that the only thing I had any control over in this scary situation was my own breastmilk. My baby was so far out of my control and we weren't even able to hold her or do anything for her at first so pumping milk became my central mothering focus. Luckily Massachusetts General Hospital (MGH) has a dedicated pair of trained lactation consultants on rotation and they showed me how to use the pump and explained very bluntly what would happen to my milk supply if I didn't follow their rigorous schedule. They put the fear in me and I pumped my colostrum and breast milk around the clock, setting my alarm to wake up every two hours through the night. The process was exhausting: assembling the pump, staying awake for the full 20 to 30 minutes of pumping, collecting and labeling the milk, cleaning all the parts and then falling asleep only to have to do it all again in 2 hours. Nevertheless I persisted and I was very lucky that my milk supply came in with no issues. After the first week of being given only IV vitamin nutrients my baby was finally well enough to be able to be fed my milk exclusively through a tiny feeding tube that went in her nose and directly down into her stomach. Luckily by then I already had amassed a good supply of frozen colostrum and milk for them to feed her

After two weeks of being intubated the breathing tube was removed and then a week later she was finally able to try breast and bottle feeding for the first time at 23 days old.When we first tried breastfeeding she surprised the nurses by being able to latch on right away but it was too tiring for her so she wasn't able to get enough milk. We worked really hard every day trying to teach her how to take all her milk orally. After 5 weeks in the NICU she was well enough to be discharged but she wasn’t strong enough or coordinated enough to get her nutritional needs met by oral feeding alone and she was still getting more than half her milk through the feeding tube at every meal. In order to get us discharged home without her needing a long term feeding tube I spent a week with her in a special rehab hospital just teaching her to drink from a bottle. It was hard work and I still had to pump every two hours to keep up my milk supply because she wasn’t able to latch and nurse efficiently herself. After a week of trial and error and really intense effort she finally understood how to effectively suck from a bottle and we were given permission to go home.

From Bottles to Breastfeeding
Once we were home I went through another intense week-long process of teaching her how to breastfeed. We began with a nipple shield and I tried many different positions to help her latch more deeply. The two most helpful tools for me were “biological or laid back nursing” and “the deep latch technique”. After several days of frustration and tons of internet research and really focused effort she learned how to nurse with a nipple shield. I remember the first time we left the house without the ball and chain of breast pumps and bottles. It was amazing. The feeling of liberation and freedom was incredible, just me and my baby out in the world living our lives! After another few days of intense effort I was able to slip the nipple shield away and have her continue nursing without it and then we were truly free, not reliant on any devices or tools, just me feeding my baby the way I had always imagined it. By the time she was two months old our nursing relationship was solid. I feel really lucky that she was able to adapt and learn a whole new way of drinking milk so many times, first the bottles, then the nipple shield and finally just my breast.
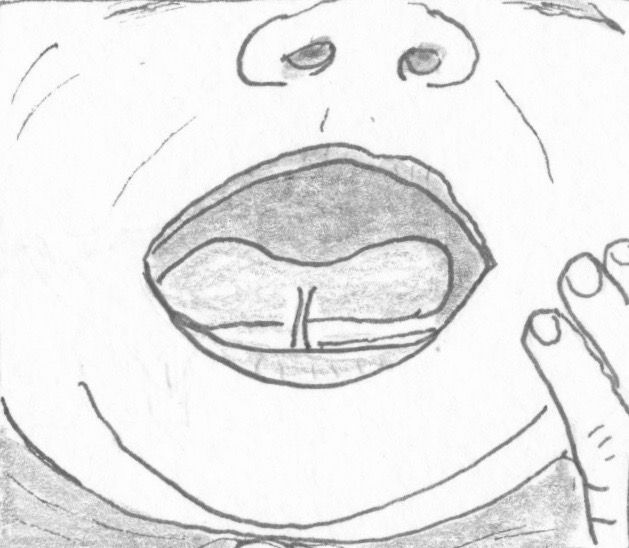
Tongue and Lip Ties
She had tongue and lip ties which had to be remediated (cut) by a specialist oral surgeon when she was four months old and after that her latch got much better and she stopped making so many gulping and clicking sounds when she nursed and she began to really gain weight. It's been smooth sailing ever since and now at 20 months old she still nurses on demand throughout the day and night. Our breastfeeding relationship is so sweet and intimate and I’m so glad that we were able to create this lovely connection after such a tough start.
Finding Emotional Closure
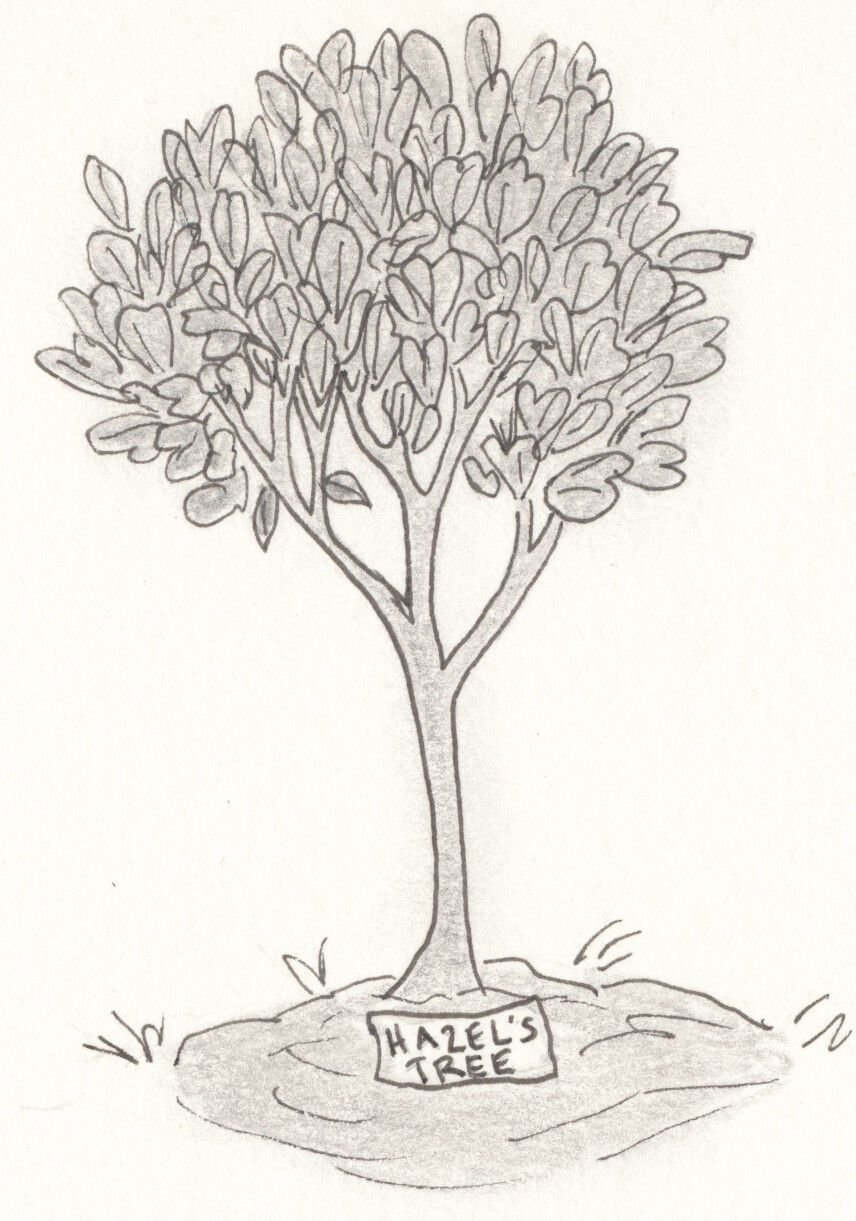
I felt so grateful to the medical community that helped my baby to survive and recover from her birth but at the same time I felt so much sadness and regret about losing the birth experience I had wanted. I had planned for and dreamed of an intimate, quiet, natural birth at home surrounded by my own familiar belongings and by people I knew and trusted. I wanted to go through the stages of labor, I wanted to experience my body doing something powerful and instinctive. I wanted to be able to reach down and feel my baby's head being born. I wanted to try being in a birthing pool and find out what that was like. I wanted to do something ceremonial and meaningful with the placenta and the umbilical cord afterwards, like plant a tree over them.
The birth experience I ended up with was the absolute opposite of that in all ways. It was invasive, stressful and full of loud medical machines beeping and the terrible sound of the doppler picking up my baby's slow, slow heartbeat. I was surrounded by people I didn't know. Because of the placental abruption my contractions were perhaps more intense and painful than they would have been at that early stage, I felt the power of my body but it felt out of control like a hurricane ripping through. I was only 5cm dilated when they took me to surgery, I never got to the pushing phase. The birth itself took place in an operating room, was 100% medicalized and extremely scary and high stakes for all involved. I was unconscious when my baby came into the world and I didn't see her at all until four hours later as she was about to be wheeled onto the helicopter. I could only see her forehead because her mouth and nose were covered in intubation tubing so I reached up from my bed and touched the side of her forehead through an opening in the incubator. Then I didn't see her again for nearly 24 hours as I waited for one of the Island's limited ambulances to become available to drive me up to Boston the next day. The Placenta and umbilical cord were sent up to Boston to be analyzed by the pathology laboratory to try to find out what had happened. When I finally tracked my placenta down several weeks later it had been entombed in formaldehyde and was given to me in a plastic bag labeled “Hazardous waste”. When I received my plastic bag full of hazardous material a sweet young medical fellow told me gently that it would be unsafe and possibly illegal to put it in the ground and plant a tree over it. This last loss brought all the other losses up in a sudden wave and the poor medical student was suddenly confronted with my despairing tears. I had been looking forward to carrying out at least one piece of my shattered birth dream and hoped to find some closure and peace through ceremony. It felt almost unbearably unfair to have had no control over my birth experience and now to lose control over what I did with my afterbirth as well.
On my baby's first birthday I had a small ceremonial tree planting and I buried the tiny piece of umbilical stump that had fallen off my baby when she was a few weeks old. It wasn't the ceremony I had envisioned but it still felt like a wound closing, like a bit of healing. I still feel great loss and sadness about the birth experience I didn't get to have. The feelings come up most often when I'm nursing my baby in the darkness in the middle of the night and my thoughts ramble. This sadness seems to be quite common among women who did not plan to have a C-section. Time does iron out the wrinkles, but at least for me I think I will always have some sadness when I think of my baby's birth.

She survived and we both healed up and time has passed and although the memories are still sharp and hurtful to think about the simple truth is that we were both so lucky to be living in the 21st century. We are so lucky to be living near a world class hospital with all the advanced medical knowledge, machines, and drugs that kept my baby alive. We are so lucky to live in a time when such highly trained specialist doctors and nurses are capable of fixing traumatic birth injuries and saving mothers and babies from the near certain death of something like a placental abruption. The gratitude and amazement never leave me. Becoming a mother has been a wonder and a joy and every day has felt simple and bright after the crazy start we had.
